Glaucoma, a group of insidious eye diseases, stands as a formidable global health challenge, damaging the optic nerve and frequently culminating in irreversible vision loss if not addressed promptly. It's a leading cause of blindness worldwide, affecting an estimated 80 million individuals globally as of 2025, with projections indicating this staggering number could swell to over 110 million by 2040. Understanding this condition – its elusive symptoms, underlying causes, precise diagnostic methods, and evolving treatments – is paramount for effective management and the preservation of sight.
The Subtle Onset: Glaucoma's Symptoms and Its Acute Manifestations
One of the most concerning aspects of glaucoma is its often asymptomatic nature in the early stages. It has rightly earned the moniker "the silent thief of sight" because most patients typically don't notice any changes in their vision until significant and, unfortunately, irreversible optic nerve damage has already occurred. This insidious progression is particularly characteristic of open-angle glaucoma, the most prevalent form of the disease.
In open-angle glaucoma, vision loss progresses slowly and painlessly, primarily affecting peripheral (side) vision. What’s more, central vision – crucial for reading, recognizing faces, and driving – is often preserved until the disease reaches its late stages. This allows the condition to advance undetected for years, making regular eye examinations critical.
In stark contrast, angle-closure glaucoma can present acutely and dramatically. Patients experiencing this form may suffer from severe eye pain, intense headaches, nausea, vomiting, blurred vision, and the unsettling sensation of seeing halos around lights. Such symptoms constitute a medical emergency requiring immediate attention to prevent rapid and profound vision loss. Other potential indicators in acute cases can include red eyes, hazy vision, and sudden visual disturbances, which should never be ignored.
Unraveling the Etiology: Causes and Risk Factors of Glaucoma
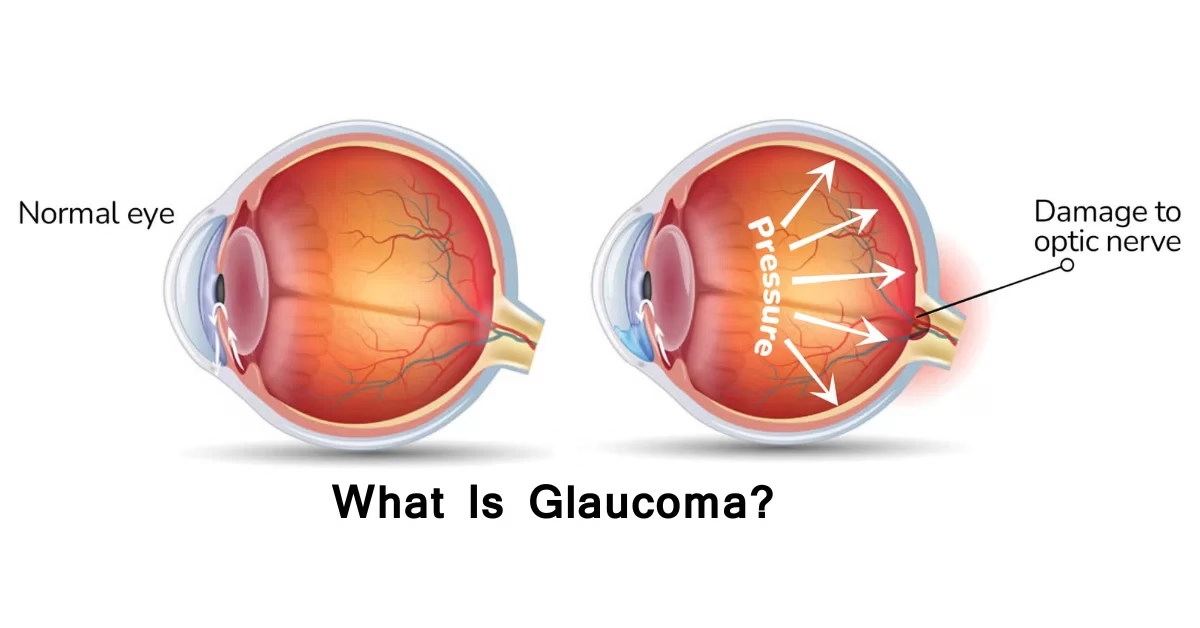
While the exact mechanisms leading to optic nerve damage in glaucoma are complex, a clear understanding of its causes and associated risk factors is crucial for prevention and early intervention. The most recognized and primary risk factor for glaucoma is elevated intraocular pressure (IOP). However, it's vital to acknowledge that glaucoma can still develop even with normal IOP, a condition known as normal-tension glaucoma, indicating other factors are at play.
Genetics play a significant role, with a family history of glaucoma substantially increasing an individual's risk. Recent genome-wide association studies have pinpointed several gene loci linked to the disease, underscoring the hereditary component. Furthermore, age is a prominent risk factor; the likelihood of developing glaucoma rises considerably after the age of 40.
Ethnicity also contributes to varying risk profiles. African, Asian, and Hispanic populations, for instance, face a higher risk for specific types of glaucoma. Beyond these primary factors, several other conditions and circumstances can heighten vulnerability. These include having thin corneas, experiencing myopia (nearsightedness), and systemic diseases such as diabetes and hypertension. Moreover, prolonged use of corticosteroids, a class of anti-inflammatory drugs, has been identified as another contributing factor.
Precision in Detection: The Diagnostic Toolkit for Glaucoma
Accurate and early diagnosis is the cornerstone of effective glaucoma management, given the irreversible nature of the vision loss it causes. A comprehensive eye examination employs several specialized tests to detect the subtle signs of optic nerve damage and elevated IOP.
Advancements in Treatment: Preserving Vision and Improving Adherence
The treatment landscape for glaucoma has seen considerable innovation, aiming to lower intraocular pressure and prevent further optic nerve damage. While vision loss cannot be restored, existing therapies are highly effective at halting or slowing progression.
Early Intervention and Adherence: Critical Factors in Glaucoma Management
The American Academy of Ophthalmology (AAO) and European Glaucoma Society (EGS) consistently underscore the paramount importance of early detection and the implementation of individualized treatment plans. Recent evidence strongly suggests that initiating treatment early, whether with SLT or prostaglandin analogs, can effectively delay or entirely prevent the progression of glaucoma in most patients. This highlights why that initial, asymptomatic phase of the disease is so critical to catch.
However, treatment adherence presents a formidable challenge in managing glaucoma. Meta-analyses from 2024–2025 reveal that a concerning proportion—up to 40%—of patients become non-adherent to their prescribed therapy within the first year. This statistic profoundly emphasizes the urgent need for enhanced patient education, improved communication from healthcare providers, and the development of simplified treatment regimens, such as the new sustained-release bimatoprost implant, to help patients stay on track.
Future Horizons and Patient Voices
The field of glaucoma management is continuously evolving, with exciting technological advances on the horizon. Beyond AI-assisted OCT analysis, emerging tools like AI-based screening and home tonometry devices hold the potential to transform future management strategies, making early detection more accessible and convenient.
Patient forums and advocacy groups, such as the Glaucoma Research Foundation and BrightFocus Foundation, reveal a mixed but understandable landscape of patient experiences. While awareness of glaucoma is on the rise, there's an ongoing undercurrent of anxiety regarding disease progression and the potential side effects of medications. Despite these concerns, many patients express significant appreciation for newer, less invasive treatments and the remarkable convenience offered by sustained-release implants. Yet, the persistent issues of cost and equitable access to these advanced therapies remain considerable concerns, particularly in low-resource settings, underscoring the need for broader healthcare solutions and support.