From Hormones to Algorithms: The Reality of Digital Contraception
For decades, reproductive health was defined by chemical intervention—pills, patches, and injections. Today, the shift is moving toward silicon and sensors. Natural Cycles remains the only FDA-cleared birth control app on the market, but its utility depends less on "tracking your period" and more on how it translates the messy biology of basal body temperature (BBT) into a mathematical model of fertility.
Unlike generic calendar apps that guess your ovulation based on a standard 28-day cycle, Natural Cycles focuses on the thermal shift triggered by progesterone. By identifying this unique spike, the system maps an individual's fertile window. However, this isn't a "set it and forget it" solution. The effectiveness of the system relies on high-quality data, and the real-world challenge is the "noise" of daily life. Fever, alcohol consumption, and irregular sleep patterns can all cause temperature fluctuations that would confuse a basic tracker. The Natural Cycles algorithm is designed to filter these outliers, though it often results in more "Red Days" (fertile days) when the data is inconsistent, requiring users to use protection or abstain.
The Wearable Ecosystem: Beyond the Thermometer
The hardware barrier was once the biggest point of friction for digital contraception. While the company still offers its proprietary NC° Band, the system’s growth is now driven by integrations with the Oura Ring and Apple Watch (Series 8 and later). This shift to passive sensing has fundamentally changed the user experience.
Instead of waking up and immediately reaching for a thermometer—a habit that many users find difficult to maintain—the integration with established wearables allows for continuous overnight temperature monitoring. This provides a much denser data set for the algorithm to analyze. For the tech-conscious user, this turns a medical requirement into a background process, though the commitment remains the same: if the watch isn't on your wrist, the system can't protect you.
Clinical Efficacy and the "Perfect Use" Gap
The numbers are well-documented: Natural Cycles carries a 93% effectiveness rate with typical use and 98% with perfect use. For context, this places it significantly higher than traditional barrier methods but requires more discipline than an IUD. It is a medical device, not a lifestyle tool, and is restricted to users 18 and older.
The platform also serves a dual purpose for those moving from prevention to family planning. The "NC° Plan Pregnancy" feature uses the same thermal data to pinpoint peak fertility, with research indicating that couples using the app conceive in an average of three cycles. To bridge the gap of "reproductive labor," the NC° Partner View allows users to sync their status with a partner, moving the responsibility of birth control away from a single individual and into a shared digital space.
The Privacy Shield in a Post-Roe Landscape
In the current legal climate, the primary concern for any digital health user is data sovereignty. Following the reversal of Roe v. Wade, the stakes for period-tracking data changed overnight. This is where the Natural Cycles subscription model moves from a business choice to a critical security feature.
While "free" apps often monetize sensitive health data to stay afloat, Natural Cycles uses its subscription revenue to maintain a "Privacy Shield" and comply with the FDA’s rigorous cybersecurity mandates. As a regulated medical device, the company is held to a higher standard of data encryption and user anonymity than a standard consumer app. Paying for the service ensures that the user remains the customer, rather than the product being sold to third-party data brokers.
A Longitudinal View of Women’s Health
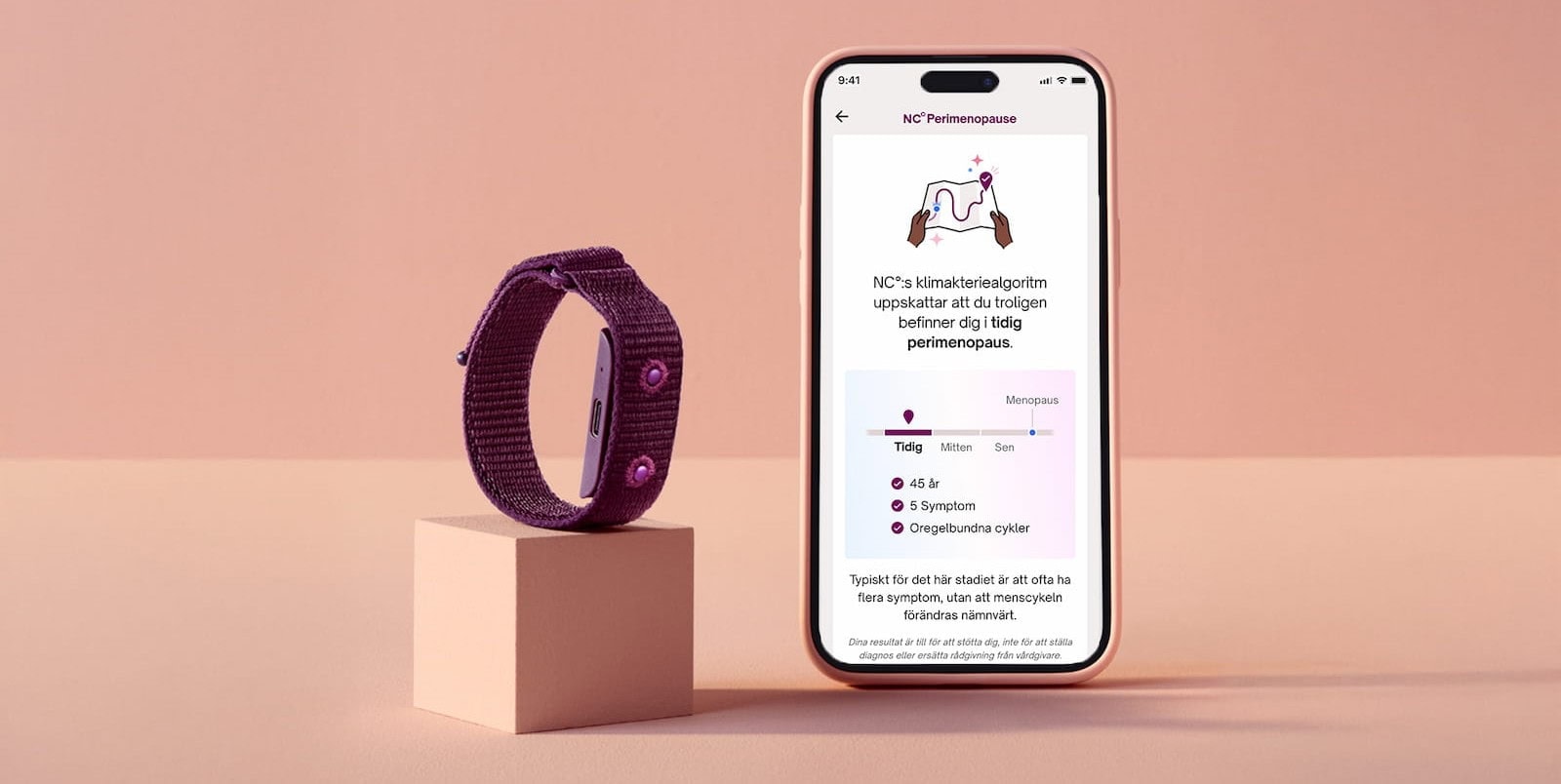
Natural Cycles has expanded its scope to cover the entire reproductive lifecycle, moving beyond simple contraception into NC° Postpartum and NC° Perimenopause. These modules address the significant hormonal shifts that occur after childbirth and during the transition to menopause—phases that are historically underserved by the med-tech industry.
By moving toward longitudinal health tracking, the platform provides a continuous record of physiological data that spans decades. As digital health tools become more integrated into standard clinical care, the distinction between a "period tracker" and a validated medical device becomes the defining factor in user safety and data integrity.